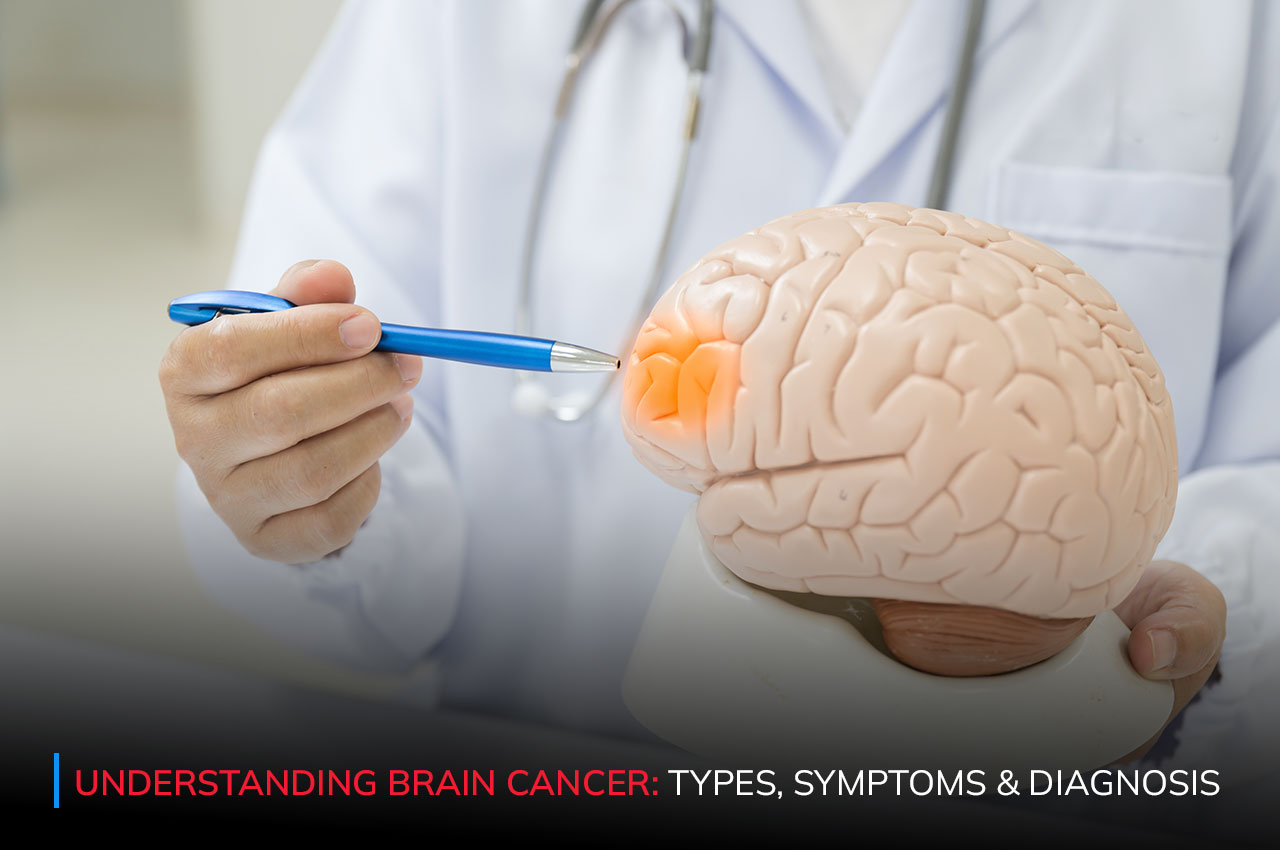
Brain cancer is a complex and challenging disease that affects thousands of individuals worldwide, with a significant impact on mortality rates. Understanding its types, symptoms, and diagnosis is crucial for early detection and effective treatment. In this comprehensive guide, we delve into the intricacies of brain cancer, shedding light on its various facets.
Brain cancer, also known as a malignant brain tumour, occurs when abnormal cells in the brain grow uncontrollably, forming a mass or tumour. These tumours can originate from brain tissue (primary brain tumours) or spread to the brain from other parts of the body (secondary or metastatic brain tumours). Primary brain tumours are classified based on the type of cells involved and their location within the brain.
Gliomas: These are primary brain tumours starting from glial cells, which support and protect neurons. They include astrocytomas, oligodendrogliomas, and ependymomas, making them the most common brain tumours.
Meningiomas: Originating from the protective membranes (meninges) around the brain and spinal cord, these tumours grow slowly and can pose challenges due to their location.
Medulloblastomas: Mostly affecting children, these tumours form in the cerebellum, impacting coordination and balance. Prompt diagnosis and treatment are crucial to address potential developmental impairments.
Pituitary Tumors: Arising from the pituitary gland at the brain’s base, these tumours can disrupt hormonal balance, leading to various symptoms and requiring specialised management.
Schwannomas: These tumours develop from Schwann cells, which support nerve fibres. They often appear along cranial or peripheral nerves and may necessitate surgical intervention to alleviate pressure on surrounding tissues.
The symptoms of brain cancer can vary depending on the tumour’s location, size, and growth rate. Common symptoms may include:
Headaches: Persistent headaches, particularly those intensifying in severity and frequency, can signal brain cancer. These headaches may not respond to typical pain relief measures and may worsen over time.
Seizures: Brain tumours can trigger seizures, which are sudden, uncontrolled electrical disturbances in the brain. Seizures may manifest as convulsions, muscle spasms, or temporary loss of consciousness.
Nausea and vomiting: Increased intracranial pressure caused by brain tumours can lead to nausea and vomiting, especially in the morning or with changes in position.
Changes in vision, hearing, or speech: Brain tumours can affect sensory and communication functions, leading to blurry or double vision, hearing loss, difficulty speaking, or slurred speech.
Weakness or numbness in the limbs: Tumors pressing on nerves or affecting brain regions controlling movement can cause weakness, numbness, or tingling sensations in the arms, legs, or face.
Cognitive changes: Brain cancer can impact cognitive abilities, resulting in memory loss, confusion, difficulty concentrating, or impaired decision-making skills.
Personality or behaviour changes: Brain tumours may influence mood and behaviour, causing irritability, mood swings, depression, or sudden changes in personality or social interactions.
It’s important to note that these symptoms can also be caused by other medical conditions, so a thorough evaluation by a healthcare professional is essential for an accurate diagnosis.
Diagnosing brain cancer typically involves a combination of imaging tests, such as MRI (magnetic resonance imaging) or CT (computed tomography) scans, to visualize the brain and identify any abnormalities. Additionally, a biopsy may be performed to obtain a sample of tissue for further analysis and confirmation of cancerous cells.
The treatment approach for brain cancer depends on several factors, including the type and stage of the tumour, as well as the patient’s overall health and preferences. Treatment modalities may include:
Surgery: Surgery is often the initial treatment for brain cancer, involving the surgical removal of the tumour. The primary goal is to excise as much of the tumour as possible while preserving neurological function. Neurosurgeons meticulously plan the procedure, considering factors such as tumour size, location within the brain, and its proximity to critical structures responsible for vital functions like movement, speech, and cognition. The extent of surgical resection varies based on these factors, to minimise the risk of tumour recurrence while ensuring optimal preservation of neurological function and quality of life for the patient.
Radiation Therapy: Radiation therapy is a crucial component of brain cancer treatment, utilising high-energy radiation beams to target and destroy cancer cells. It can be employed as the primary treatment modality for tumours that are inoperable or located in sensitive areas where surgery carries significant risks. Additionally, radiation therapy may be used in combination with surgery and/or chemotherapy to enhance treatment efficacy by eradicating any remaining cancer cells. This approach is particularly beneficial for reducing the risk of tumour recurrence and improving overall patient outcomes. By precisely delivering radiation to the tumour site, this treatment minimises damage to surrounding healthy brain tissue, thereby reducing the risk of adverse effects.
Chemotherapy: Chemotherapy involves the administration of anti-cancer drugs, either orally or intravenously, to impede the growth and spread of cancer cells. Unlike surgery and radiation therapy, which target specific areas of the brain, chemotherapy works systematically, circulating throughout the body to reach cancer cells wherever they may be located. This makes it particularly useful for treating tumours that are difficult to access surgically or have spread beyond the primary site. Chemotherapy is often used in combination with other treatment modalities to maximise its effectiveness and improve patient outcomes.
Targeted Therapy: Targeted therapy is a precision medicine approach that specifically targets cancer cells while minimising damage to healthy cells. Unlike traditional chemotherapy, which can affect rapidly dividing cells indiscriminately, targeted therapy acts on specific molecular pathways or proteins that are essential for cancer cell survival and proliferation. By blocking these targets, targeted therapy inhibits tumour growth and progression. This approach offers the potential for enhanced treatment efficacy with fewer side effects compared to conventional chemotherapy. Targeted therapy is often used in combination with other treatments, such as surgery, radiation therapy, or chemotherapy, to achieve optimal outcomes for patients with brain cancer.
Early detection of brain cancer is critical for improving treatment outcomes and patient survival rates. Recognising the warning signs and seeking prompt medical attention can lead to timely diagnosis and intervention, potentially preventing the disease from advancing to a more advanced stage.
At PBHRC Elgin Road Clinic, our commitment lies in delivering comprehensive and personalised care to individuals battling brain cancer. Our team of healthcare professionals, spanning various disciplines, employs state-of-the-art diagnostic tools and evidence-based treatments to achieve optimal patient outcomes. We take pride in our reliance on research-backed therapies, focusing on non-invasive methods to minimise adverse effects and expedite recovery.
Emphasising the significance of early detection, we vigilantly identify warning signs, enabling timely intervention. With a legacy of four generations and over 150 years of homoeopathic expertise, PBHRC embodies trust in healthcare. We prioritise accessibility through both in-person and virtual consultations, ensuring affordability with competitive pricing and complimentary services for the less privileged. In our relentless fight against brain cancer, we uphold a holistic approach, dedicated to enhancing patient well-being and fostering a brighter tomorrow.